Publication: ASCO 2023, Abstract TPS615
Authors
Elise Deluche, Stefan Michiels, Daniele Fric, Christophe Perrin, Caroline Bailleux, Thomas Bachelot, Pascal Ko Kivok Yun, Gaetan De Rauglaudre, Marie-Ange Mouret-Reynier, Romauld Le Scodan, Ines Vaz-Luis, Magali Lacroix-Triki, Clara Guyonneau, Fabrice Andre
Organizations
Centre Hospitalier Universitaire, Limoges, France, Office of Biostatistics and Epidemiology, Gustave Roussy, Villejuif, France, Groupe Hospitalier Mutualiste de Grenoble, Grenoble, France, Centre Eugène Marquis, Rennes, France, Centre Antoine Lacassagne, Nice, France, Medical Oncology, Centre Léon Bérard, Lyon, France, Centre Hospitalier International, Mont De Marsan, France, Institut du cancer Sainte-Catherine, Avignon, France, Centre Jean Perrin, Clermont-Ferrand, France, St. Gregoire Private Hospital Centre, Saint-Gregoire, France, Breast Cancer Survivorship Group, INSERM Unit 981, Gustave Roussy, Villejuif, France, Gustave Roussy, Villejuif, France, R&D UNICANCER, French Breast Cancer Intergroup, Paris, France, Institut Gustave Roussy, Villejuif, France
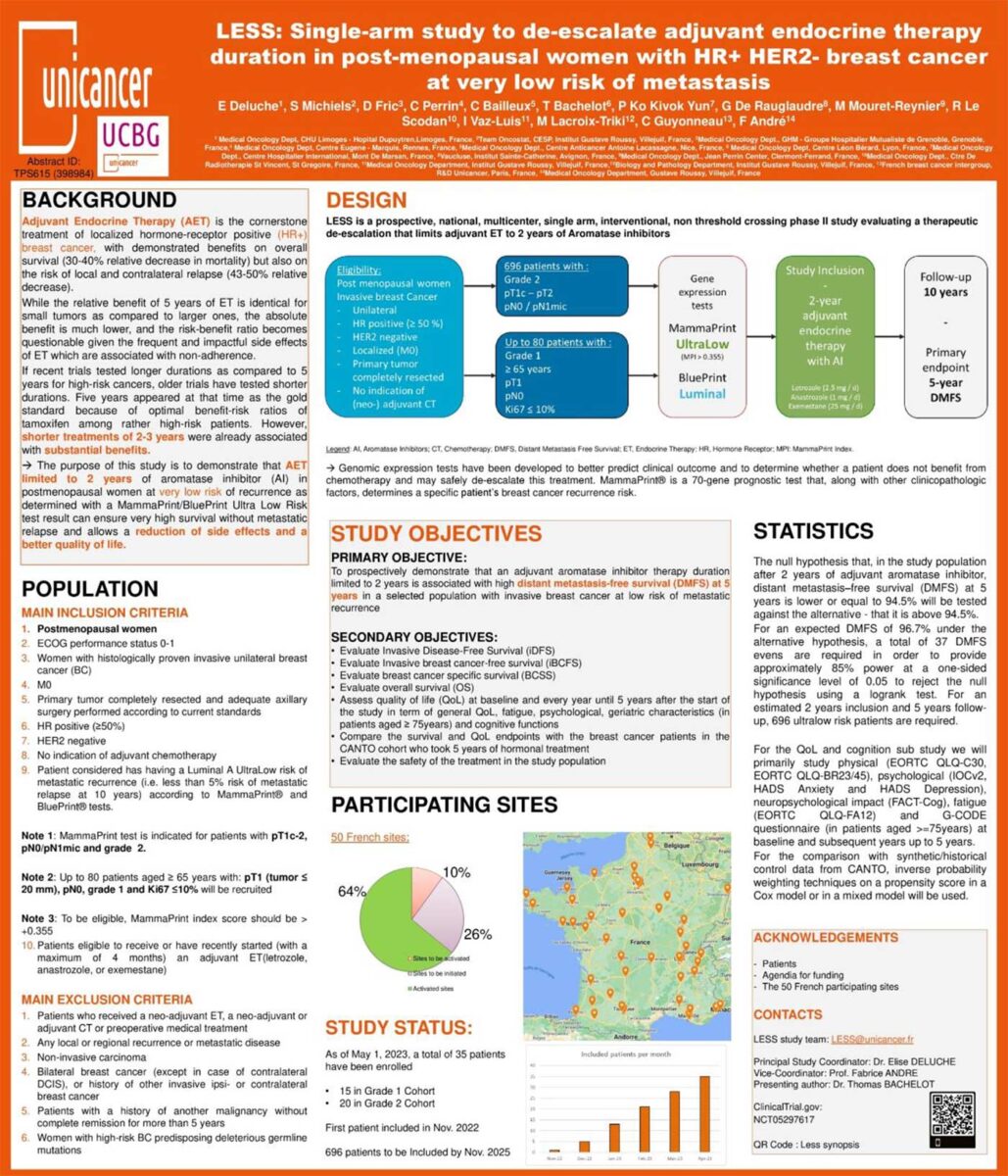
Background & Objective
Adjuvant Endocrine Therapy (ET) is the cornerstone treatment of localized hormone-receptor positive (HR+) breast cancer, with demonstrated benefits on overall survival (30-40% relative decrease in mortality) but also on the risk of local and contralateral relapse (43-50% relative decrease). While the relative benefit of 5 years of ET is identical for small tumors as compared to larger ones, the absolute benefit is much lower, and the risk-benefit ratio becomes questionable given the frequent and impactful side effects of ET which are associated with non-adherence. If recent trials tested longer durations as compared to 5 years for high-risk cancers, older trials have tested shorter durations. Five years appeared at that time as the gold standard because of optimal benefit-risk ratios of tamoxifen among rather high-risk patients. However, shorter treatments of 2-3 years were already associated with substantial benefits and may be enough for very low risk patients.
The purpose of this study is to demonstrate that adjuvant ET limited to 2 years of aromatase inhibitor (AI) in postmenopausal women at very low risk of recurrence as determined with a MammaPrint and BluePrint Ultra Low Risk Luminal test result can ensure very high survival without metastatic relapse and allows a reduction of side effects and a better quality of life.
Methods
LESS (NCT05297617) is a prospective, national, multicenter, single-arm, interventional, non-threshold crossing phase II study evaluating a therapeutic de-escalation that limits adjuvant ET to 2 years of AI. Approximately 696 post-menopausal patients with an invasive unilateral, HR+, HER2-negative, without indication of adjuvant chemoT and genomically-assessed MammaPrint/BluePrint UltraLow risk Luminal A breast cancer tumors, will be enrolled. LESS will include two sub cohorts: the majority of patients with Grade 2, pT1c-2, pN0/N1mic tumors, and up to 80 patients ≥65 years with Grade 1, pT1, pN0 and Ki67<10% tumors.
The primary endpoint is distant metastasis free survival (DMFS) defined as the time from date of registration to date of first event of distant recurrence, death, or second primary non-breast invasive cancer. Secondary endpoints include the assessment of quality of life parameters and psychological aspects related to this de-escalation. The null hypothesis (H0) that, in the study population after 2 years of adjuvant AI, DMFS at 5 years is lower or equal to 94.5% will be tested against the alternative – that it is above 94.5%. For an expected DMFS of 96.7% under the alternative hypothesis, a total of 37 DMFS events are required in order to provide approximately 85% power at a one-sided significance level of 0.05 to reject H0 using a logrank test. The 1st patient was included in October 2022, initiating the 2-year inclusion period and 10 years FU per patient. Clinical trial information: NCT05297617.
References and Acknowledgments
Patients
Agendia for funding
The 50 French participating sites
Study Status:
As of May 1, 2023, a total of 35 patients have been enrolled
- 15 in Grade 1 Cohort
- 20 in Grade 2 Cohort
First patient included in Nov. 2022
696 Patients to be included by Nov. 2025


