OUR TESTS
BluePrint – Molecular Subtyping Test

What’s driving the growth of my patient’s breast cancer?
Interrogating 80 genes, the BluePrint® test identifies the underlying biology of an individual breast cancer. The tumor is then accurately classified as one of three subtypes, which reveal valuable information about its behavior, long-term prognosis and response to systemic therapy. Results are typically available in <6 days, just in time for your pre-operative consultation.1,2

I am a strong believer in treating a patient’s breast cancer according to the subtype of their cancer. We should not treat all breast cancers the same.
– Dr. Peter Beitsch, MD
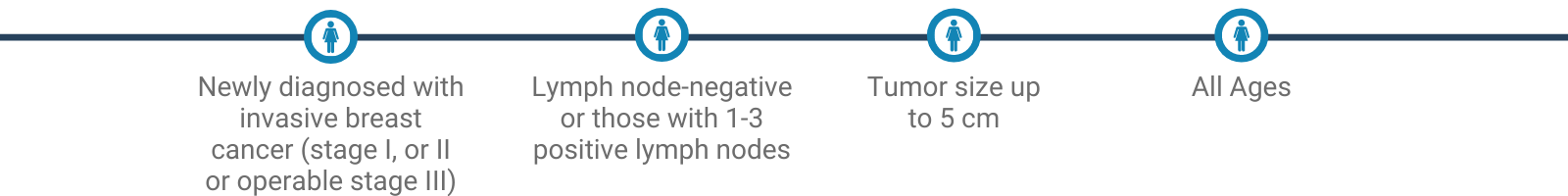
Women who benefit.
Reclassification
ER+/BASAL PATIENTS ARE
BluePrint Basal-Type
MAMMAPRINT HIGH RISK
Clinically, these patients appear to have less aggressive tumors but the underlying biology indicates they will act like triple negative breast cancer.2 Treating ER+/Basal patients more aggressively may improve their outcomes.
ER+, HER2+/LUMINAL PATIENTS ARE
BluePrint/Luminal-Type
MAMMAPRINT HIGH RISK
Nearly 50% of pathologically HER2+ patients are reclassified to a Luminal molecular subtype. ER+, HER2+/Luminal patients do not respond as well to treatment with HER2-targeted agents as those who have concordant clinical and molecular HER2 subtypes.3
In the NBRST study, 22% of patients were reclassified from their original clinical or pathologic subtype into a different molecular subtype identifying an opportunity to personalize treatment to the patient’s molecular profile.4
The MammaPrint + BluePrint Test Suite
The potential to go even deeper. To treat even more effectively.
With the combined insights of MammaPrint and BluePrint alongside clinical factors, physicians gain a more comprehensive basis for predicting prognosis and the benefit of specific treatments.
MammaPrint enables us to further divide luminal tumors into two subtypes that align with the test’s binary results.

1. BluePrint is a laboratory-developed test that was developed, validated and is performed exclusively by Agendia. The test is intended for clinical purposes. The test has not been cleared by the U.S. Food and Drug Administration (FDA) but has been CE-marked for use in Europe. The laboratory is regulated under the Clinical Laboratory Improvement Amendments (CLIA) to ensure the quality and validity of the tests. Our laboratories are CAP-accredited and certified under CLIA to perform high complexity clinical laboratory testing. (Agendia is committed to delivering results in less than 10 business days, and results are provided within 6 business days for the majority of cases)
2. Groenendijk FH, et al. NPJ Breast Cancer. 2019;5:15.
3. Rong P et. al. Cancer Res 2018;78(13 Suppl):Abstract nr 2612.
4. Whitworth, et al. Ann Surg Oncol (2017) 24:669–675
1. BluePrint is a laboratory-developed test that was developed, validated and is performed exclusively by Agendia. The test is intended for clinical purposes. The test has not been cleared by the U.S. Food and Drug Administration (FDA) but has been CE-marked for use in Europe. The laboratory is regulated under the Clinical Laboratory Improvement Amendments (CLIA) to ensure the quality and validity of the tests. Our laboratories are CAP-accredited and certified under CLIA to perform high complexity clinical laboratory testing. (Agendia is committed to delivering results in less than 10 business days, and results are provided within 6 business days for the majority of cases)
2. Groenendijk FH, et al. NPJ Breast Cancer. 2019;5:15.
3. Rong P et. al. Cancer Res 2018;78(13 Suppl):Abstract nr 2612.
4. Whitworth, et al. Ann Surg Oncol (2017) 24:669–675


