Publication: ASCO 2023, Abstract #564
Authors
Sonya Reid1, Tuya Pal1, Xiao-Ou Shu1, Lindsay Venton1, Jennifer G. Whisenant1, Kent Hoskins2, Eduardo Dias3, Rakhshanda Layeequr Rahman4, Jennifer Wei5, Ciera Singleton5, Sahra Uygun5, Andrea Menicucci5, Patricia Dauer5, and William Audeh5
1Department of Medicine, Vanderbilt University Medical Center, Nashville, TN; 2Division of Hematology/Oncology, University of Illinois at Chicago, Chicago, IL; 3Nashville Breast Center, Nashville, TN; 4Texas Tech University, Lubbock, TX; 5Agendia Inc., Irvine, CA
Background & Objective
- Breast cancer (BC) is the leading cause of cancer-related deaths in Black women, who are 41% more likely to die from BC than White women1.
- We’ve recently reported that Black women have a significantly greater proportion of hormone receptor-positive (HR+) tumors further classified as Basal-Type with BluePrint genomic subtyping, which may contribute to their worse outcomes2,3.
- Here, we evaluated whether there were differences in tumor genomics among patients with clinically assessed HER2+ (cHER2) tumors between Black and White women.
Methods
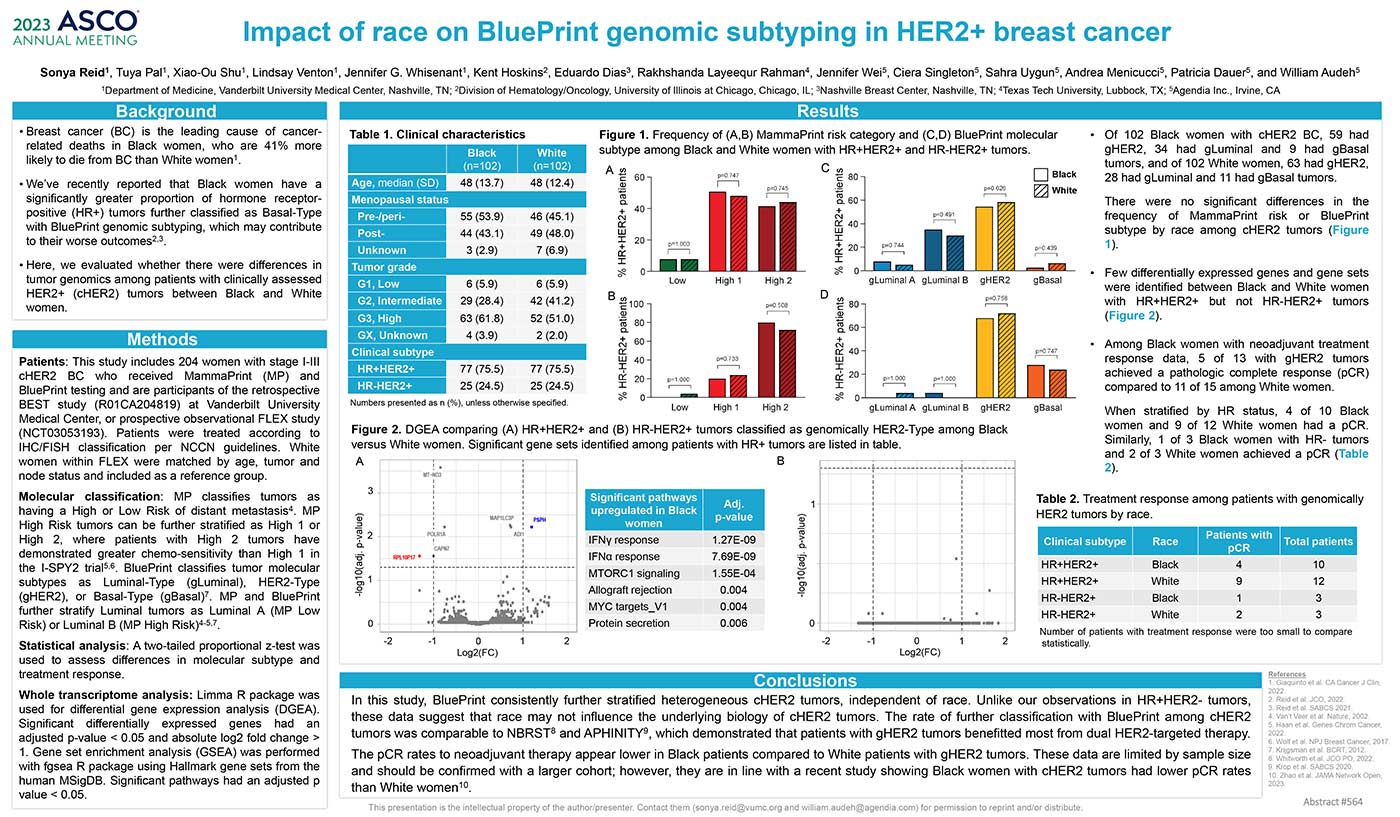
Patients: This study includes 204 women with stage I-III cHER2 BC who received MammaPrint (MP) and BluePrint testing and are participants of the retrospective BEST study (R01CA204819) at Vanderbilt University Medical Center, or prospective observational FLEX study (NCT03053193). Patients were treated according to IHC/FISH classification per NCCN guidelines. White women within FLEX were matched by age, tumor and node status and included as a reference group.
Molecular classification: MP classifies tumors as having a High or Low Risk of distant metastasis4. MP High Risk tumors can be further stratified as High 1 or High 2, where patients with High 2 tumors have demonstrated greater chemo-sensitivity than High 1 in the I-SPY2 trial5,6. BluePrint classifies tumor molecular subtypes as Luminal-Type (gLuminal), HER2-Type (gHER2), or Basal-Type (gBasal)7. MP and BluePrint further stratify Luminal tumors as Luminal A (MP Low Risk) or Luminal B (MP High Risk)4-5,7.
Statistical analysis: A two-tailed proportional z-test was used to assess differences in molecular subtype and treatment response.
Whole transcriptome analysis: Limma R package was used for differential gene expression analysis (DGEA). Significant differentially expressed genes had an adjusted p-value < 0.05 and absolute log2 fold change > 1. Gene set enrichment analysis (GSEA) was performed with fgsea R package using Hallmark gene sets from the human MSigDB. Significant pathways had an adjusted p value < 0.05.
Results
- Of 102 Black women with cHER2 BC, 59 had gHER2, 34 had gLuminal and 9 had gBasal tumors, and of 102 White women, 63 had gHER2, 28 had gLuminal and 11 had gBasal tumors.
There were no significant differences in the frequency of MammaPrint risk or BluePrint subtype by race among cHER2 tumors (Figure 1).
- Few differentially expressed genes and gene sets were identified between Black and White women with HR+HER2+ but not HR-HER2+ tumors (Figure 2).
- Among Black women with neoadjuvant treatment response data, 5 of 13 with gHER2 tumors achieved a pathologic complete response (pCR) compared to 11 of 15 among White women.
When stratified by HR status, 4 of 10 Black women and 9 of 12 White women had a pCR. Similarly, 1 of 3 Black women with HR- tumors and 2 of 3 White women achieved a pCR (Table 2).
Conclusion:
In this study, BluePrint consistently further stratified heterogeneous cHER2 tumors, independent of race. Unlike our observations in HR+HER2- tumors, these data suggest that race may not influence the underlying biology of cHER2 tumors. The rate of further classification with BluePrint among cHER2 tumors was comparable to NBRST8 and APHINITY9, which demonstrated that patients with gHER2 tumors benefitted most from dual HER2-targeted therapy.
The pCR rates to neoadjuvant therapy appear lower in Black patients compared to White patients with gHER2 tumors. These data are limited by sample size and should be confirmed with a larger cohort; however, they are in line with a recent study showing Black women with cHER2 tumors had lower pCR rates than White women10.
References and Acknowledgments
1. Giaquinto et al. CA Cancer J Clin, 2022.
2. Reid et al. JCO, 2022.
3. Reid et al. SABCS 2021.
4. Van’t Veer et al. Nature, 2002.
5. Haan et al. Genes Chrom Cancer, 2022.
6. Wolf et al. NPJ Breast Cancer, 2017.
7. Krijgsman et al. BCRT, 2012.
8. Whitworth et al. JCO PO, 2022.
9. Krop et al. SABCS 2020.
10. Zhao et al. JAMA Network Open, 2023.


