Publication: SABCS 2025, Presentation ID: PS5-04-19
Authors: Cobain et al.
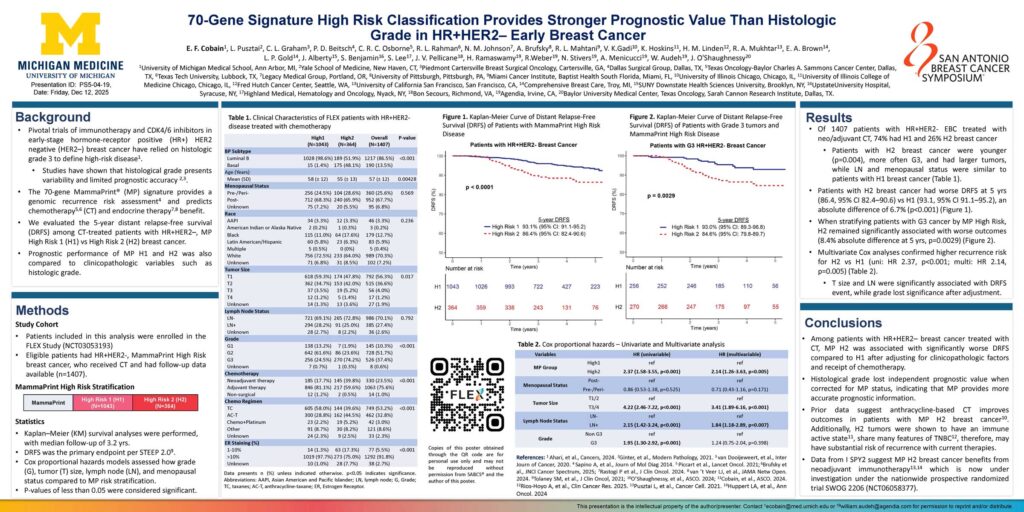
Title: Improved 3-year IDFS with anthracycline-based therapy for patients with 70-gene signature High 2, Luminal B, HR+HER2- early-stage breast cancer
Introduction:
- Pivotal trials of immunotherapy and CDK4/6 inhibitors in early-stage hormone-receptor positive (HR+) HER2 negative (HER2–) breast cancer have relied on histologic grade 3 to define high-risk disease1.Studies have shown that histological grade presents variability and limited prognostic accuracy.
- The 70-gene MammaPrint® (MP) signature provides a genomic recurrence risk assessment4 and predicts chemotherapy (CT) and endocrine therapy benefit.
- We evaluated the 5-year distant relapse-free survival (DRFS) among CT-treated patients with HR+HER2–, MP High Risk 1 (H1) vs High Risk 2 (H2) breast cancer.
- Prognostic performance of MP H1 and H2 was also compared to clinicopathologic variables such as histologic grade.
Methods:
- Patients included in this analysis were enrolled in the FLEX Study (NCT03053193)
- Eligible patients had HR+HER2-, MammaPrint High Risk breast cancer, who received CT and had follow-up data available (n=1407).
Results:
- Of 1407 patients with HR+HER2- EBC treated with neo/adjuvant CT, 74% had H1 and 26% H2 breast cancer Patients with H2 breast cancer were younger (p=0.004), more often G3, and had larger tumors, while LN and menopausal status were similar to patients with H1 breast cancer (Table 1).
- Patients with H2 breast cancer had worse DRFS at 5 yrs (86.4, 95% CI 82.4–90.6) vs H1 (93.1, 95% CI 91.1–95.2), an absolute difference of 6.7% (p<0.001) (Figure 1).
- When stratifying patients with G3 cancer by MP High Risk, H2 remained significantly associated with worse outcomes (8.4% absolute difference at 5 yrs, p=0.0029) (Figure 2).
- Multivariate Cox analyses confirmed higher recurrence risk for H2 vs H1 (uni: HR 2.37, p<0.001; multi: HR 2.14, p=0.005) (Table 2).T size and LN were significantly associated with DRFS event, while grade lost significance after adjustment.
Conclusions:
- Among patients with HR+HER2– breast cancer treated with CT, MP H2 was associated with significantly worse DRFS compared to H1 after adjusting for clinicopathologic factors and receipt of chemotherapy.
- Histological grade lost independent prognostic value when corrected for MP status, indicating that MP provides more accurate prognostic information.
- Prior data suggest anthracycline-based CT improves outcomes in patients with MP H2 breast cancer10. Additionally, H2 tumors were shown to have an immune active state11, share many features of TNBC12, therefore, may have substantial risk of recurrence with current therapies.
- Data from I SPY2 suggest MP H2 breast cancer benefits from neoadjuvant immunotherapy13,14 which is now under investigation under the nationwide prospective randomized trial SWOG 2206 (NCT06058377).