PUBLICATION: ASCO 2021
Authors
Nina D’Abreo1,2, Abhinav Rohatgi1,2, Douglas Kanter Marks1,2, Heather M. Kling3, Josien Haan4, William Audeh3, FLEX Investigators Group5
Background
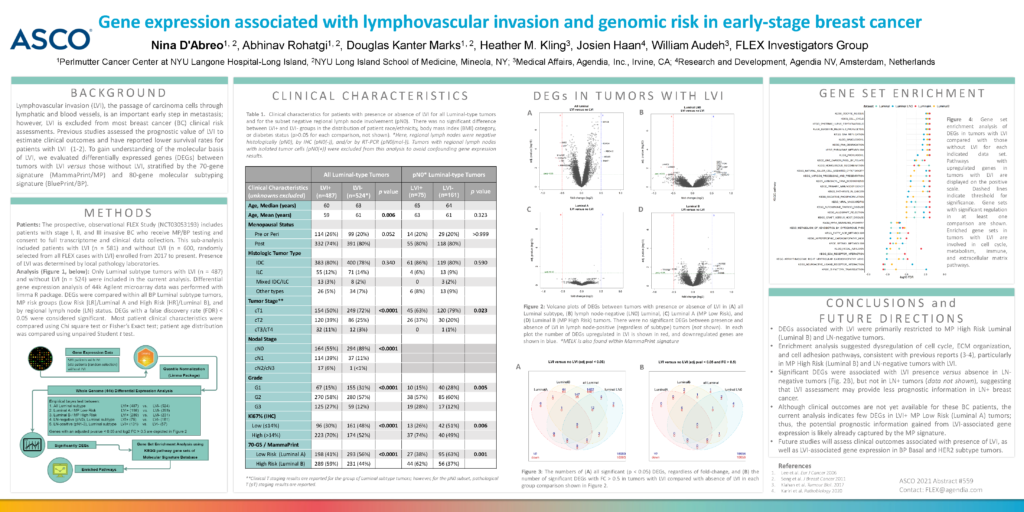
Lymphovascular invasion (LVI), the passage of carcinoma cells through lymphatic and blood vessels, is an important early step in metastasis; however, LVI is excluded from most breast cancer (BC) clinical risk assessments. Previous studies assessed the prognostic value of LVI to estimate clinical outcomes and have reported lower survival rates for patients with LVI (1-2). To gain understanding of the molecular basis of LVI, we evaluated differentially expressed genes (DEGs) between tumors with LVI versus those without LVI, stratified by the 70-gene signature (MammaPrint/MP) and 80-gene molecular subtyping signature (BluePrint/BP).
Methods
Patients: The prospective, observational FLEX Study (NCT03053193) includes patients with stage I, II, and III invasive BC who receive MP/BP testing and consent to full transcriptome and clinical data collection. This sub-analysis included patients with LVI (n = 581) and without LVI (n = 600, randomly selected from all FLEX cases with LVI) enrolled from 2017 to present. Presence of LVI was determined by local pathology laboratories.
Analysis (Figure 1, below): Only Luminal subtype tumors with LVI (n = 487) and without LVI (n = 524) were included in the current analysis. Differential gene expression analysis of 44k Agilent microarray data was performed with limma R package. DEGs were compared within all BP Luminal subtype tumors, MP risk groups (Low Risk [LR]/Luminal A and High Risk [HR]/Luminal B), and by regional lymph node (LN) status. DEGs with a false discovery rate (FDR) < 0.05 were considered significant. Most patient clinical characteristics were compared using Chi square test or Fisher’s Exact test; patient age distribution was compared using unpaired Student t test.
Conclusions and Future Direction
- DEGs associated with LVI were primarily restricted to MP High Risk Luminal (Luminal B) and LN-negative tumors.
- Enrichment analysis suggested dysregulation of cell cycle, ECM organization, and cell adhesion pathways, consistent with previous reports (3-4), particularly in MP High Risk (Luminal B) and LN-negative tumors with LVI.
- Significant DEGs were associated with LVI presence versus absence in LN-negative tumors (Fig. 2B), but not in LN+ tumors (data not shown), suggesting that LVI assessment may provide less prognostic information in LN+ breast cancer.
- Although clinical outcomes are not yet available for these BC patients, the current analysis indicates few DEGs in LVI+ MP Low Risk (Luminal A) tumors; thus, the potential prognostic information gained from LVI-associated gene expression is likely already captured by the MP signature.
- Future studies will assess clinical outcomes associated with presence of LVI, as well as LVI-associated gene expression in BP Basal and HER2 subtype tumors.
1. Perlmutter Cancer Center at NYU Langone Hospital-Long Island, 2. NYU Long Island School of Medicine, Mineola, NY; 3. Medical Affairs, Agendia, Inc., Irvine, CA; 4. Research and Development, Agendia NV, Amsterdam, Netherlands 5. FLEX Investigators’ Group