PUBLICATION:
SABCS 2020
AUTHORS:
Beth-Ann Lesnikoski, Jennifer A. Crozier, Gordan Srkalovic, Patricia Robinson, Clodia Osipo, Kalyan Banda, Heather M. Kling, Midas M. Kuilman, Josien Haan, William Audeh, and FLEX Investigators Group
Background:
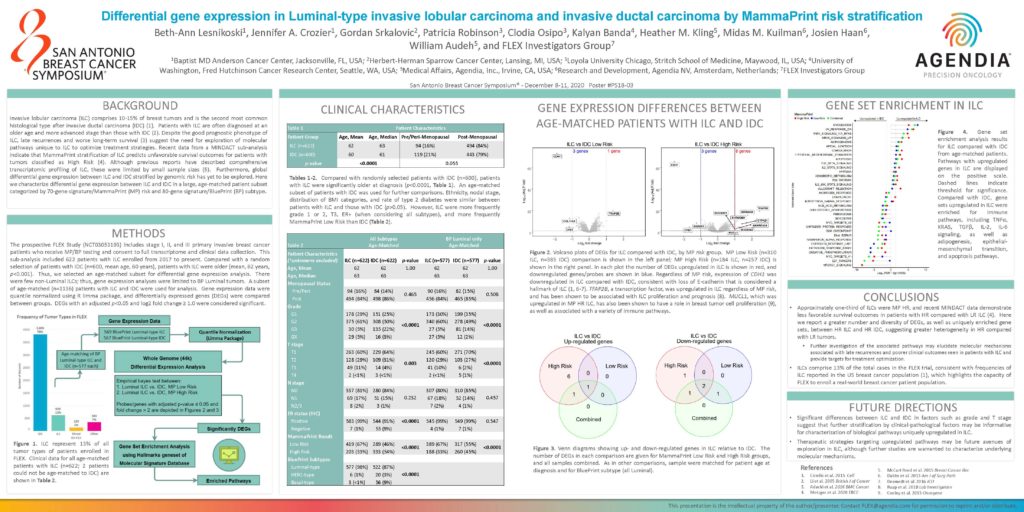
Invasive lobular carcinoma (ILC) comprises 10-15% of breast tumors and is the second most common histological type after invasive ductal carcinoma (IDC) (1). Patients with ILC are often diagnosed at an older age and more advanced stage than those with IDC (2). Despite the good prognostic phenotype of ILC, late recurrences and worse long-term survival (3) suggest the need for exploration of molecular pathways unique to ILC to optimize treatment strategies. Recent data from a MINDACT sub-analysis indicate that MammaPrint stratification of ILC predicts unfavorable survival outcomes for patients with tumors classified as High Risk (4). Although previous reports have described comprehensive transcriptomic profiling of ILC, these were limited by small sample sizes (5). Furthermore, global differential gene expression between ILC and IDC stratified by genomic risk has yet to be explored. Here we characterize differential gene expression between ILC and IDC in a large, age-matched patient subset categorized by 70-gene signature/MammaPrint (MP) risk and 80-gene signature/BluePrint (BP) subtype.
Methods
The prospective FLEX Study (NCT03053193) includes stage I, II, and III primary invasive breast cancer patients who receive MP/BP testing and consent to full transcriptome and clinical data collection. This sub-analysis included 622 patients with ILC enrolled from 2017 to present. Compared with a random selection of patients with IDC (n=600, mean age, 60 years), patients with ILC were older (mean, 62 years, p<0.001). Thus, we selected an age-matched subset for differential gene expression analysis. There were few non-Luminal ILCs; thus, gene expression analyses were limited to BP Luminal tumors. A subset of age-matched (n=1136) patients with ILC and IDC were used for analysis. Gene expression data were quantile normalized using R limma package, and differentially expressed genes (DEGs) were compared between groups. DEGs with an adjusted p<0.05 and log2 fold change ≥ 1.0 were considered significant.
Conclusions
- Approximately one-third of ILCs were MP HR, and recent MINDACT data demonstrate less favorable survival outcomes in patients with HR compared with LR ILC (4). Here we report a greater number and diversity of DEGs, as well as uniquely enriched gene sets, between HR ILC and HR IDC, suggesting greater heterogeneity in HR compared with LR tumors.
- Further investigation of the associated pathways may elucidate molecular mechanisms associated with late recurrences and poorer clinical outcomes seen in patients with ILC and provide targets for treatment optimization.
- ILCs comprise 13% of the total cases in the FLEX trial, consistent with frequencies of ILC reported in the US breast cancer population (1), which highlights the capacity of FLEX to enroll a real-world breast cancer patient population.