Publication: ESMO BREAST CANCER CONGRESS 2022
Authors
De Lameillieure K (1), Van der Meijden C (1), Klinkhamer J (1) , Cusumano P (2).
1- Medical & Clinical Affairs, Agendia NV., Amsterdam, Netherlands, 2 – Breast Clinic, Centre Hospitalier Chrétien, Liège, Belgium
Background & Objective
Gene expression profiling (GEP) tests, including the MammaPrint® 70-gene signature, are used to support treatment decisions for patients with early-stage breast cancer, such as to identify those with a genomic Low Risk who may safely forgo chemotherapy. 1,2
Currently, the impact of GEP tests on the final treatment strategy of physicians in Belgium is being investigated in a pilot study, sponsored by INAMI-RIZIV. 3 Within this pilot, patients with clinical high-risk early breast cancer, with HR+, HER2- tumors and up to 3 positive lymph nodes have access to MammaPrint.
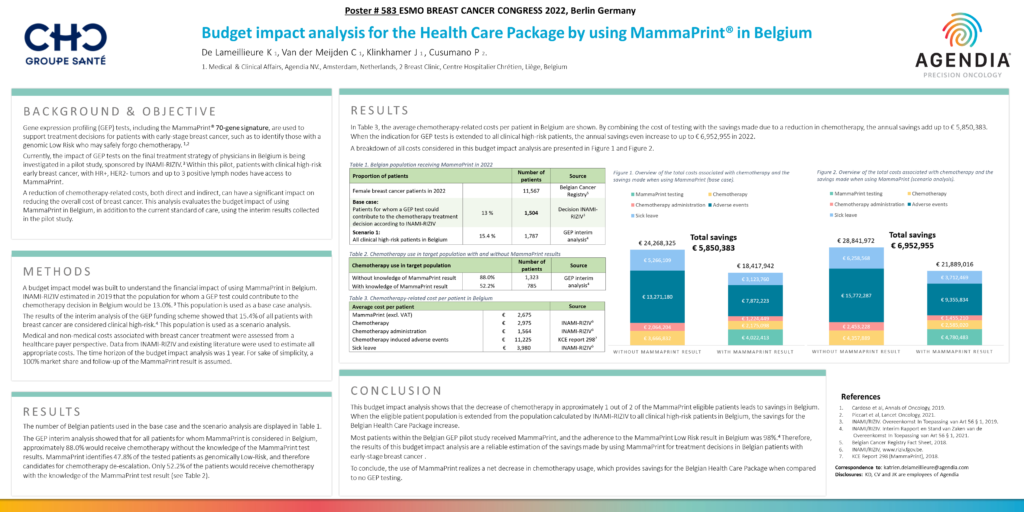
A reduction of chemotherapy-related costs, both direct and indirect, can have a significant impact on reducing the overall cost of breast cancer. This analysis evaluates the budget impact of using MammaPrint in Belgium, in addition to the current standard of care, using the interim results collected in the pilot study.
Methods
A budget impact model was built to understand the financial impact of using MammaPrint in Belgium. INAMI-RIZIV estimated in 2019 that the population for whom a GEP test could contribute to the chemotherapy decision in Belgium would be 13.0%. 3 This population is used as a base case analysis.
The results of the interim analysis of the GEP funding scheme showed that 15.4% of all patients with breast cancer are considered clinical high-risk.4 This population is used as a scenario analysis.
Medical and non-medical costs associated with breast cancer treatment were assessed from a healthcare payer perspective. Data from INAMI-RIZIV and existing literature were used to estimate all appropriate costs. The time horizon of the budget impact analysis was 1 year. For sake of simplicity, a 100% market share and follow-up of the MammaPrint result is assumed.
Results
The number of Belgian patients used in the base case and the scenario analysis are displayed in Table 1.
The GEP interim analysis showed that for all patients for whom MammaPrint is considered in Belgium, approximately 88.0% would receive chemotherapy without the knowledge of the MammaPrint test results. MammaPrint identifies 47.8% of the tested patients as genomically Low-Risk, and therefore candidates for chemotherapy de-escalation. Only 52.2% of the patients would receive chemotherapy with the knowledge of the MammaPrint test result (see Table 2).
Conclusion
This budget impact analysis shows that the decrease of chemotherapy in approximately 1 out of 2 of the MammaPrint eligible patients leads to savings in Belgium. When the eligible patient population is extended from the population calculated by INAMI-RIZIV to all clinical high-risk patients in Belgium, the savings for the Belgian Health Care Package increase.
Most patients within the Belgian GEP pilot study received MammaPrint, and the adherence to the MammaPrint Low Risk result in Belgium was 98%.4 Therefore, the results of this budget impact analysis are a reliable estimation of the savings made by using MammaPrint for treatment decisions in Belgian patients with early-stage breast cancer .
To conclude, the use of MammaPrint realizes a net decrease in chemotherapy usage, which provides savings for the Belgian Health Care Package when compared to no GEP testing.
References and Acknowledgments
- Cardoso et al, Annals of Oncology, 2019.
- Piccart et al, Lancet Oncology, 2021.
- INAMI/RIZIV. Overeenkomst In Toepassing van Art 56 § 1, 2019.
- INAMI/RIZIV. Interim Rapport en Stand van Zaken van de Overeenkomst In Toepassing van Art 56 § 1, 2021.
- Belgian Cancer Registry Fact Sheet, 2018.
- INAMI/RIZIV, www.riziv.fgov.be.
- KCE Report 298 (MammaPrint), 2018.


