PUBLICATION:
SABCS 2020
AUTHORS:
Dipali Sharma, Lisa E. Blumencranz, Heather M. Kling, Sahra Uygun, Sarah Untch, William Audeh, Jennifer A. Crozier, Mehran Habibi, and Raquel Nunes
Background:
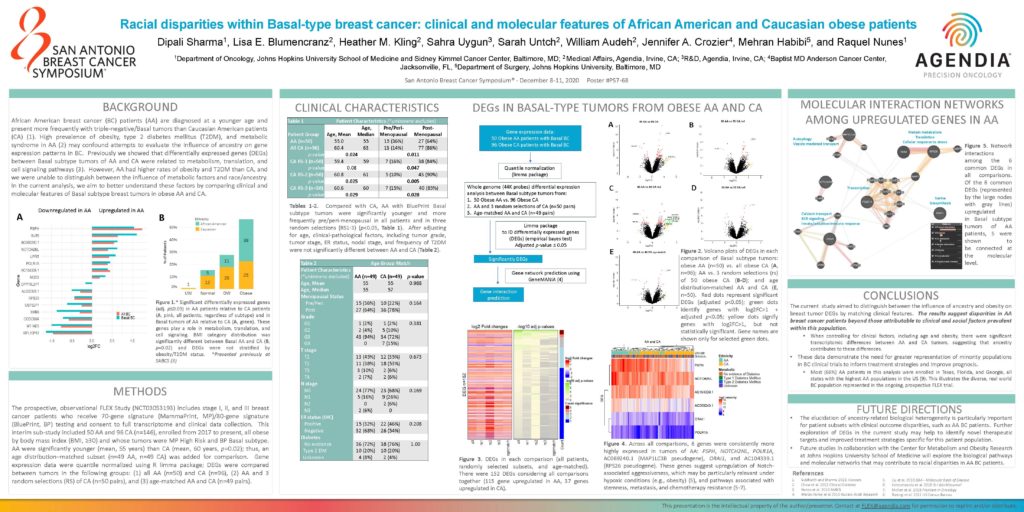
African American breast cancer (BC) patients (AA) are diagnosed at a younger age and present more frequently with triple-negative/Basal tumors than Caucasian American patients (CA) (1). High prevalence of obesity, type 2 diabetes mellitus (T2DM), and metabolic syndrome in AA (2) may confound attempts to evaluate the influence of ancestry on gene expression patterns in BC. Previously we showed that differentially expressed genes (DEGs) between Basal subtype tumors of AA and CA were related to metabolism, translation, and cell signaling pathways (3). However, AA had higher rates of obesity and T2DM than CA, and we were unable to distinguish between the influence of metabolic factors and race/ancestry. In the current analysis, we aim to better understand these factors by comparing clinical and molecular features of Basal subtype breast tumors in obese AA and CA.
Methods
The prospective, observational FLEX Study (NCT03053193) includes stage I, II, and III breast cancer patients who receive 70-gene signature (MammaPrint, MP)/80-gene signature (BluePrint, BP) testing and consent to full transcriptome and clinical data collection. This interim sub-study included 50 AA and 96 CA (n=146), enrolled from 2017 to present, all obese by body mass index (BMI, ≥30) and whose tumors were MP High Risk and BP Basal subtype. AA were significantly younger (mean, 55 years) than CA (mean, 60 years, p=0.02); thus, an age distribution–matched subset (n=49 AA, n=49 CA) was added for comparison. Gene expression data were quantile normalized using R limma package; DEGs were compared between tumors in the following groups: (1) all AA (n=50) and CA (n=96), (2) AA and 3 random selections (RS) of CA (n=50 pairs), and (3) age-matched AA and CA (n=49 pairs).
Conclusions
- The current study aimed to distinguish between the influence of ancestry and obesity on breast tumor DEGs by matching clinical features. The results suggest disparities in AA breast cancer patients beyond those attributable to clinical and social factors prevalent within this population.
- When controlling for clinical factors, including age and obesity, there were significant transcriptomic differences between AA and CA tumors, suggesting that ancestry contributes to these differences.
- These data demonstrate the need for greater representation of minority populations in BC clinical trials to inform treatment strategies and improve prognosis.
- Most (66%) AA patients in this analysis were enrolled in Texas, Florida, and Georgia, all states with the highest AA populations in the US (9). This illustrates the diverse, real world BC population represented in the ongoing, prospective FLEX trial.
Future Directions
- The elucidation of ancestry-related biological heterogeneity is particularly important for patient subsets with clinical outcome disparities, such as AA BC patients. Further exploration of DEGs in the current study may help to identify novel therapeutic targets and improved treatment strategies specific for this patient population.
- Future studies in collaboration with the Center for Metabolism and Obesity Research at Johns Hopkins University School of Medicine will explore the biological pathways and molecular networks that may contribute to racial disparities in AA BC patients.