Source: San Antonio Breast Cancer Symposium® 2024
Authors: Joyce O’Shaughnessy, Priyanka Sharma, Cynthia R C Osborne, Gregory Vidal, Pond Remsen Kelemen, Suzanne Hoekstra, Harshini Ramaswamy, Nicole Stivers, Andrea Menicucci, William Audeh, FLEX Investigators’ Group
Title: MammaPrint® and BluePrint® Predict Pathological Response to Neoadjuvant Chemotherapy in Patients With HR+HER2- Early-Stage Breast Cancer Enrolled in FLEX
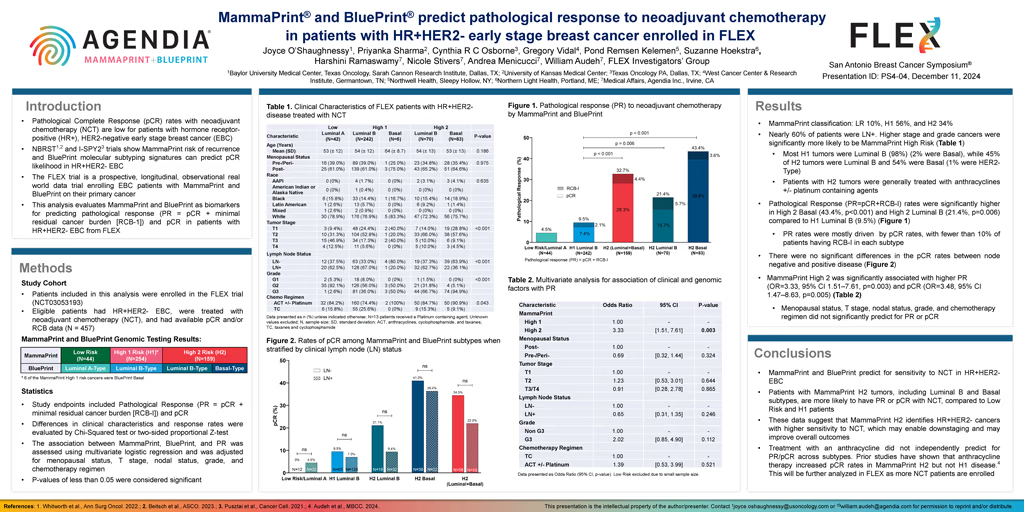
Background: For patients with hormone receptor-positive (HR+), HER2-negative early-stage breast cancer (EBC), pathological Complete Response (pCR) rates to neoadjuvant chemotherapy (NCT) are low. However, NBRST and I-SPY2 trials report that MammaPrint risk of distant recurrence and BluePrint molecular subtyping signatures can more accurately identify which HR+HER2- EBC patients are likely to achieve pCR. Here, MammaPrint and BluePrint as biomarkers for predicting pCR and residual cancer burden (RCB) class, was evaluated among patients with HR+HER2- tumors enrolled in FLEX.
Methods: Patients with HR+HER2- tumors treated with NCT with available pCR and/or RCB data enrolled in the ongoing prospective, observational FLEX Trial (NCT03053193), were included in this study (N = 457). Tumors were characterized as MammaPrint UltraLow (UL), Low (LR), High 1 (H1) or High 2 (H2) Risk. BluePrint subtypes were classified as either Luminal A, Luminal B, HER2, or Basal. pCR and Pathological Response (PR= pCR + minimal residual cancer burden [RCB-I]) were the study endpoints. Differences in clinical characteristics and response rates were evaluated by Chi-Squared test or two-sided proportional Z-test. The association between MammaPrint, BluePrint, and PR was assessed using multivariate logistic regression and was adjusted for menopausal status, T stage, and N stage.
Results: MammaPrint classified 2% as UL, 8% as LR, 56% as H1, and 34% as H2. Nearly 60% of patients in this study had clinical lymph node (LN) positive disease. Higher tumor stage and grade were significantly more likely to be associated with higher MammaPrint Risk. Age, menopausal status, race, and LN status were comparable among MammaPrint groups. All UL and LR tumors were Luminal A, most H1 tumors were Luminal B (98%), while 45% of H2 tumors were Luminal B and 54% were Basal (1% were HER2). pCR rates were significantly higher in H2 Basal (39.8%), followed by H2 Luminal B (15.7%), H1 Luminal B (7.4%), and lowest in UL and LR, Luminal A (4.5%) (p<0.001). Among H2 Luminal B tumors, LN negative tumors had a pCR rate of 21.0% whereas LN positive tumors had a pCR rate of 12.5%. Rates of RCB-I were significantly higher among H2 tumors (26.9%) than H1 tumors (7.3%), or UL and LR tumors (0%) (p=0.026). Among H2 tumors, PR rates measured higher than rates of pCR alone in Basal tumors (43.4% vs 39.8%) and more prominently in Luminal B tumors (21.4% vs. 15.7%). Multivariate analysis revealed that MammaPrint H2 was significantly associated with likelihood of PR (OR=12.6, 95% CI 2.43 – 23.28, p=0.016), whereas menopausal status, T stage, and N stage were not associated with PR.
Conclusion: MammaPrint and BluePrint predict chemosensitivity to NCT in HR+HER2- EBC. Patients with MammaPrint H2 tumors, including Luminal B and Basal subtypes, are more likely to achieve pCR or PR to NCT, compared to UL, LR, and H1 groups. Additionally, pCR rates trended lower among LN positive disease, possibly due to the increased difficulty of clearing disease in LNs with systemic therapy. We observed very high rates of RCB-I in H2 Luminal B tumors. These findings should be confirmed in other studies. The very high rates of PR observed in this study suggest that MammaPrint H2 identifies a subset of patients with HR+HER2- disease that benefit from NCT, which may enable surgical downstaging efforts and translate to improvements in outcomes.