
By Kris Conner | August 7, 2024
How the diagnostic test MammaPrint empowered Laura-Lynn to find answers and advocate to improve the quality of her life.
In the summer of 2020, Laura-Lynn Renner, a seasoned financial advisor from Sparks, Maryland, faced a stage I breast cancer diagnosis that upended her world during the COVID-19 pandemic.
Determined to navigate her treatment journey with the same care and thought she devoted to her career, Laura-Lynn did research and asked questions to inform her treatment choices. After she struggled with difficult side effects from tamoxifen, she discovered that a MammaPrint test could help her make an informed decision about whether or not she needed to continue with hormonal therapy.
LBBC’s frequent contributor Kris Conner spoke with Laura-Lynn to learn more about how she found both the confidence and the information she needed to make decisions about her care.
You were diagnosed soon after the nation shut down due to COVID-19. What was that like?
In spring 2020, I discovered a lump in my left breast. Within a few days, I found myself sitting in a surgeon’s office as she explained my treatment options for stage I, estrogen receptor-positive breast cancer.
Hospitals were overwhelmed with COVID patients, and there was real fear that surgeries would be delayed or even halted altogether. Still, I managed to schedule a lumpectomy within three weeks.
Since my husband could not accompany me, I spent a lot of time sitting in exam rooms by myself. Masked. Naked under my thin gown. Vulnerable.
What helped you get through it?
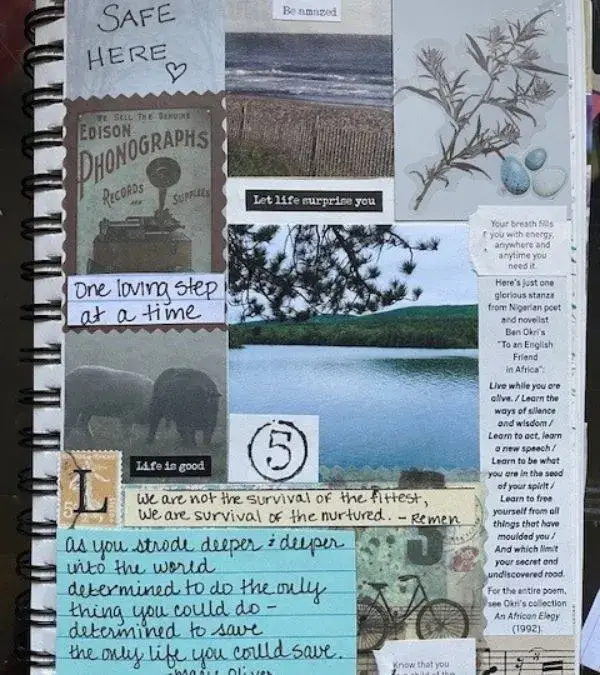
It was many things. Mindfulness techniques that I’d learned the year before really helped me cope as I sat alone in those exam rooms, and so did meditation, deep breathing, and art journaling. I started by adopting a mantra to get from one moment to the next and stuck to it. “One loving step at a time,” I would tell myself in the face of each new challenge.

What was your treatment plan, and when did you start hormonal therapy?
I had a no-nonsense female surgeon and radiologist who were true partners in my care. They patiently answered my long list of questions and provided the information I needed to make the right choices for me. After my lumpectomy, an OncotypeDX test showed that my cancer had a low risk of recurrence, so I wouldn’t need chemo. I completed accelerated partial breast irradiation and headed to a medical oncologist.
I went into that appointment with another long list of questions. Right away, the doctor told me our visit would be brief because the path was clear: I would need to take tamoxifen for five years. I didn’t get to ask my questions, but I like to make well-informed decisions. I asked how long I could reasonably wait before starting tamoxifen, and she said three months.
I used that time to do more research and prepare my body to start. I wanted a full picture of my health before tamoxifen. I found a naturopathic doctor who ordered baseline bloodwork and other tests, and we worked on my nutrition.
I lost weight, walked two miles every day, took a hard look at making changes at my stressful job, prioritized sleep, stepped up my meditation, and met with my therapist via Zoom. All during a global pandemic while supporting my clients through a volatile stock market! I faltered, got messy, occasionally broke down, and rested when necessary, but I kept taking each day one loving step at a time.
What was your experience with tamoxifen like, and what led you to the MammaPrint test?
About a month into it, I started feeling intense side effects, and the list only seemed to grow. The worst were the daily body pain and restless legs syndrome. The only thing that helped was walking, and I logged two or three miles a few times a day, even though I didn’t have a ton of energy.
By this time, I was seeing a different oncologist, as the first one had moved out of state. Each time I mentioned that the side effects were becoming more intolerable, she offered a new prescription to combat them, but I didn’t want to keep adding more medicines. Other remedies I read about for menopausal symptoms were contraindicated with tamoxifen. I kept pushing forward.
After two-and-a-half years with a diminishing quality of life, I wondered if there was some way to determine whether there was still a benefit to continuing tamoxifen. I do know tamoxifen is helpful for a lot of women, but I happened to be someone who really struggled with it. I’ve always reacted strongly to medications; it’s just how my body is.
In March 2023, I came across an article about MammaPrint and learned that it’s a genomic test that can help doctors decide if post-menopausal women with early-stage breast cancer need the full five years of hormonal therapy. I saw the test was included in the updated National Comprehensive Cancer Network Guidelines, so it’s recommended by the leading cancer experts.
Since I was post-menopausal by then, I was super excited and asked my oncologist about the test. She told me it was expensive, not yet part of standard practice, and my insurance wouldn’t pay for it. I said I would pay out of pocket if I had to, but she resisted and said I should just stop taking the tamoxifen if I couldn’t tolerate it. But I only wanted to do that if I knew it was the right choice.
I sent the article and research about MammaPrint to my general practitioner, who thought I was a good candidate and agreed to order it for me. I then reached out to Agendia, the company that developed this test, and learned it had to be ordered by an oncologist or surgeon. The representative at Agendia helped me better understand the test and encouraged me to get a second opinion with another oncologist more familiar with MammaPrint.

“’One loving step at a time,’ I would tell myself in the face of each new challenge.”
What was the testing process like?
The second opinion was helpful as the doctor explained everything, and I listened carefully. I learned that only an “ultralow” score identified patients who could safely stop hormonal therapy before five years while still maintaining excellent survival. If the result came back as “low” but not “ultralow,” research suggested that continuing hormonal therapy for seven years might be beneficial for me. (Editor’s note: Each person’s case is individual, and a score of “low” may not always mean that it would be helpful for a person to extend hormonal therapy to seven years.)
There was a possibility that I wouldn’t like the test results. Still, I wanted the information to be sure I was making the best decision for me.
The doctor requested my tumor sample be sent to Agendia for the test. My insurance company paid for it without issue, and it cost me $300 out of pocket, which was reasonable given the decline in my quality of life. A few weeks later, I got a call from the doctor. The results were ultralow! I jumped up and down in happiness.
After receiving the report, I felt comfortable stopping the tamoxifen and continuing regular follow-ups with my breast surgeon, along with yearly mammograms.
It’s been a year now, and any side effects are completely gone. My energy is better, the body pain has vanished, and the crazy-high anxiety has ceased. I recently celebrated my four-year clear mammogram. I also retired from my high-stress job in December. In addition to art journaling, I’m a big knitter, I garden, and I’m teaching myself watercolor.
I’m glad that I advocated for myself and my body, and I got my life back. My advice would be to ask questions and do research using credible sources.
What other advice would you give to people who are juggling breast cancer with other stressors and trying to advocate for themselves?
Seek out a therapist you trust and can be completely honest with. My therapist taught me to say, “Good job, Laura-Lynn!” after each step of treatment. She helped me to realize that my body wasn’t the enemy—that it was merely trying to survive and handle all the stress that life entails. I added the mantra, “Same team, same team, same team.” I would write these and other mantras on post-it notes and leave them on my computer.
Learn meditation. An app like Insight Timer can give you free, easy access from your phone. Walk, eat well, look at your sleep hygiene, engage in a creative hobby, get out in nature.
We must be able to befriend our bodies, be mindful of our thoughts and speak to ourselves with kindness, so if we find ourselves in an empty exam room, we don’t feel alone and are able to find the energy to take one loving step a time.

See the original article here.


